PEDS CNS: Crainiopharyngioma
Background
Craniopharyngiomas are epithelial tumors arising from the remenants of Rathke's pouch in the suprasellar region. They are benign tumors.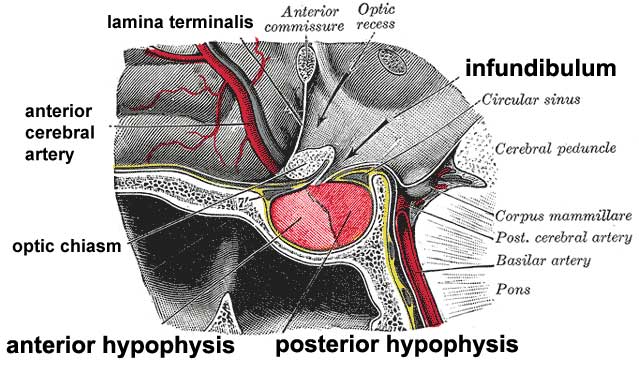
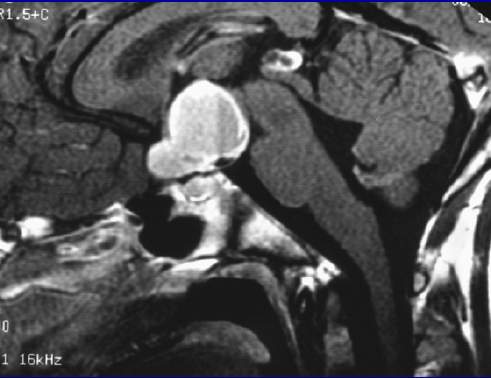
The typical craniopharyngioma is calcified, cystic tumor derived from embryonic cell rests of enamel organs found adjacent to and along the pituitary stalk. The cysts are filled with high lipid content fluid frequently referred to as "crankcase oil"
Less common squamous cell type craniopharygiomas more frequently and almost exclusively occur in adults.
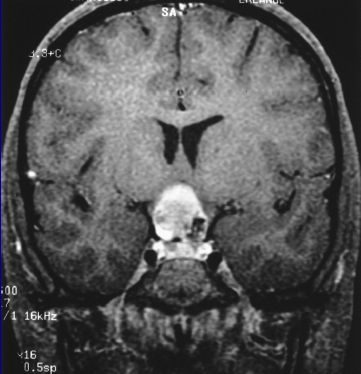
Crainiopharyngiomas are well circumscribed, encapsulated extra-axial lesions with intergigitating patters of adhesion to adjacent neurologic structures including the optic chiasm, the major vessels of the Circle of Willis, the tuber cinerum of the pituitary stalk and the hypothalamus. Craniopharyngiomas are graded on the basis of invasiveness of the hypothalamus:
- none/no invasion of hypothalamus
- abutting/displacing hypothalamus
- involving/infiltrating (absense of hypothalamus on imaging)
Anatomically 70-90% involve the retrochiasmatic region, extending superiorly into the third ventricle. Children often present with visual disturbances with impaired acuity or field cuts along with symptoms of increased intracranial pressure. About 50% - 90% also present with endocrine deficits, most often decreased growth hormone, diabetes insipitus, and decreasted gonadotropin or ACTH. Personality changes and altered cognition are also noted in up to 50% of children at presentation.
Craniopharyngiomas most frequently arise in the suprasellar region, or the sella proper (less common). Although benign, they become problematic due to local progression around critical structures. Tumors becme increasingly problematic due to their spatial location, abutting the third ventricle causing increased intracranial pressure.
Demographics
There are about 300 - 350 cases annually in the US. The median age at diagnosis is 5 - 10 years. The highest risk age is < 20 years and > 40 years. The distribution is bimodal.1/3 will occur in patients age 0 - 14 years.
Pathology
There are two histological subtypes, the adamantinomatous subtype, found most frequently in children and the squamous subtype found almost exclusively in adults.
Adamantinoumatous craniopharyngiomas have a solid and cystic pattern with the cysts filled with "machine oil." This oil filled cyst can change rapidly with treatment so frequent on-treatment imaging is mandatory.
At presentation, Growth hormone deficiencies are the most common hormonal disturbance.
Craniopharyngiomas can be calcified or non-calcified. Non-calcified craniopharyngiomas provide the best prognosis.
As benign tumors, craniopharyngiomas respond very slowly to radiation therapy.
Workup and Staging
Craniopharyngioma workup includes an history and physical examination, basic laboratories, pituitary panel and MRI of the brain. In addition, ancillary studies must be performed:
- Endocrine panel
- audiometry
- vision including fields of view
- neuropsychiatric studies
Craniopharyngiomas appear as partially calcified and cystic lesions on CT and MRI. Biopsy confirmation is not absolutely necessary for the diagnosis of craniopharyngiomas. Diagnosis can be made based on imaging findinga and cystic fluid analysis. There is no formal staging other than the degree of grading based on th amount of hypothalamic invasion.
 |
 |
Treatment and Prognosis
The general treatment paradigm for craniopharyngioma is
- Maximum safe surgical resection
- External beam radiation therapy with intracystic chemotherapy either at resection or at recurrence.
Surgery
Surgical approaches encompass a lateral temporal craniotomy. Observation after incomplete resection may be employed and is especially appropriate in younger patients. Adjvant and salvage therapy may have similar local control in closely followed patients. Tomita (2005 Childs Nerv syst) reports 20 -3 % of all attempted gross total resections result in only a subtotal resection.
The LC-10 for surgery alone (GTR + STR cases) is 42%. Adding radiation to surgery improves LC-10 to 84% (Stripp IJROBP 2004). However, radiation therapy may be reserved as salvage therapy since salvage radiation therapy yields the same ten year local control as adjuvant radiation therapy.
Chemotherapy
Craniopharyngioma cysts can be managed with surgical aspiration, bleomycin injection or radioisotope injection. Bleomycin has been typically used for intracystic chemotherapy. With limited data, there appears to be about an overall response rate to intracystic bleomycin of 65%.
Radiotherapy
External Beam Radiation Therapy
External beam radiation therapy has been used as post-op treatment both adjuvant and salvage to good effect increasing the LC-10 from 41% to around 84%. Radiation is delivered to a total dose of 54 Gy with EBRT or alternatively 12- 14 Gy SRS.
The GTV consists of the decompressed/post-operative volume of tumor + cyst wall. PTV = GTV+ 1 1.5 cm margin. There is no CTV in this set up.
Isotope Therapy
A number of β emitting isotopes are used to deliver intracystic radiation therapy:
- 90Y
- 32P
- 186Rh
The overall dose to the cystic wall is 200 Gy - 250 Gy. P-32 is conjugated to a large sugar molecule to keep the agent within the cyst. The preservative in the P-32 suspension is sodium benzoate which is a neurotoxin, thus the need to keep P-32 sequestered in the cyst. P-32 has a mean β energy of 0.7 MeV, and a T1/2 of 2 weeks. the effective depth of penetration is 3 mm - 4 mm.
The indications for intralesional cyst management are cyst volume > 50% of total tumor bulk and the number of cysts is ≤ 3.
Patients may have worsening visual signs during radiation therapy. Acute symptoms/exacerbations are not due to acute side effects of radiation therapy. They are due to a rapidly enlarging cystic component. In this situation, urgen surgical intervention is indicated for cystic decompression. Some (U.FL, Wayne State/GROC) advocate serial MRIs during radiation therapy.
The typical response to intralesional brachytherapy is 80% with stable or improving visual symptoms in 51%. Median survival is 9 years.
Factors associated with inferior control include lesions > 5 cm and radiation dose < 55 Gy based on U. Pitt. data, 2002, IJROBP. Cystic regrowth may occur after radiation therapy, but these tumors respond slowly to radiation and radiation therapy can take a long time to affect the tumors. Repeat aspirations are in order if symptoms develop.
The OS-5 for craniopharyngioma is 80%. The long term survival OS-20 is 60%. For recurrent lesions, the OS-20 drops to 25%.
A French Study by Puget in 2007 (J. Neurosurg.) . showed significant reductions in endocrine and hypothalamic dysfunction if patients were prospectively stratified into degree of hypothalamic involvement:
- Grades 0 - 1: Attempt GTR
- Grades 2: STR + Radiation therapy if age > 5 years; otherwise, if age < 5 years post-op observation only.
If tumors regrow, there is much variability in time to recurrence. The average time is 2 years, but regrowth can occur up to 9 years. Long term follow up is essential with serial MRIs and close neuro-opthalmologic and endocrine exams.
Toxicities
Vision loss occurs in < 2%. Hypopituitism and hypothalamic injury causing hypothalamic eating disorders, defective short term memory, sleep disturbances.
Radiation therapy side effects in the treatment of craniopharyngioma include the standard concerns: cognitive dysfunction, loss of 10% IQ, endocrine dysfunction, secondary late malignancy, cystic enlargement, and vasculopathy.
Surgical mortality can be as high as 10%. Because of this, STR + radiation therapy = GTR, in terms of outcomes. Radical surgery is not mandatory. In addition, St. Jude data showed that hte surgery group also lost an averge 9.8 points IQ, while the STR + radiation therapy group only lost 1.25 IQ points.
Diabetes Insipitus is the most common surgical morbidity of craniopharyngioma while radiation induced diabetes insipitus is rare. Radiation's most common morbidity is Growth Hormone reduction.