PEDS CNS: Brainstem Gliomas
Background
Brainstem gliomas compromise 10% of pediatric CNS tumors, but < 2% of adult tumors. The peak age of brainstem gliomas is 5 years to 9 years with a slight male predominance. There are two classes of brainstem gliomas:
- Focal Brainstem gliomas (30% of brainstem gliomas) involve more commonly the upper midbrain and lower medulla and carry the best prognosis.
- Diffuse brainstem gliomas (70%) are most commonly found in the pons and upper midbrain, are infiltrative and carry the worst prognosis.
Brainstem gliomas in the medulla are most commonly glioblastoma multiforme. They are most commonly high grade astrocytoma (Grade III) disease in the midbrain. Childhood brainstem gliomas have a worse prognosis than adult brainstem gliomas since they are high grade more often children than in adults. Adult brainstem gliomas are mainly low grade.
Prognosis
The median survival for brainstem gliomas is not good. Overall the disease is lethal in > 90%. The specific median survivals by group are:
- Adults: 7.3 years
- Children: 1 year
- Elderly: 11 months
Workup and Staging
Presentation
Brainstem gliomas typically present with new onset neurologic symptoms rapidly. The general findings for diffuse pontine gliomas include:
- CN palsy, involving VI (abducens causing lateral gaze deviation/convergent strabismus and diplopia), VII
- Ataxia
- Long tract signs including hyperreflexia.
Suspected brainstem glioma is an imaging workup. No biopsy is required and should not be performed due to the risk of morbidity. The standard H&P, labs and MRI are used.
Biopsy
Biopsy of the brainstem is risky, When imaging can confirm a typical appearance, the MRI is diagnostic. However, when there is an atypical clinical course, or an unusual MRI appearance, indicating a potential alternative diagnosis, such as a benign tumor or infectious etiology, then a biopsy may be appropriate.
There is no formal staging for brainstem gliomas.
Treatment
The standard treatment paradigm for brainstem gliomas include starting steroids and inserting a shunt for increased intracranial pressure. This is followed by radiation therapy alone ± temazolamide (on study).
The dorsal exophytic brainstem gliomas are potentially amenable to surgical resection ± adjuvant radiation therapy. Dorsal exophytic brainstem gliomas have an OS-10 with surgery ± radiation therapy of 75%. Most of these tumors are juvenile pilocytic astrocytomas (JPA) with a good prognosis.
Chemotherapy
There is no demonstrable benefit to chemotherapy in brainstem gliomas. There is very minimal response with single, combination or high dose chemotherapy with stem cell rescue.
Temozolomide is presently the subject of study in brainstem gliomas. There is no indication for temozolomide after completion of radiaiton therapy in this group. Concurrent temozolomide is presently under study in a COG Phase II trial.
Radiation Therapy
Radiation therapy for brainstem gliomas is to 54 Gy at 1.8 Gy/fraction. 2/3 of the brainstem gliomas will have stablization after treatment or improvement in symptoms.
There is no evidence to support a role for hypofractionation. POG/CCG studies in multiple trials failed to show an improvment with hyperfractionation. There was better radiologic response at higher doses, which was offset by greater radionecrosis and long term steroid dependancy.
There is no known role for gamma knife radiosurgery in the treatment of brainstem gliomas.
Tectal Plate Tumors
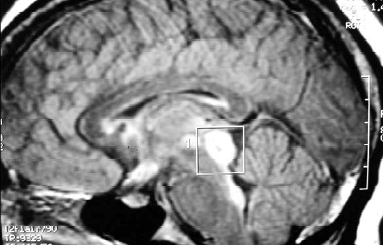 |
Tectal plate tumors are generally managed with observation and VP shunt if necessary. These are typically indolent juvenile pilocytic astrocytomas.
Prognosis
The major prognostic factors are:
- diffuse or focal
- child (MS 1 year) or adult (MS 7.3 years)
- histology
Diffuse brainstem glioma heralds poor survival with a 12 month median survival and occurs more frequently in children and accounts for 30% of the upper midbrain tumors. Focal disease accounts for the balance and carries an OS-10 of 50% - 70%.
Toxicity
Dose limits to the brainstem are 54 Gy EBRT at standard fractionation and 12 Gy @ 1 fraction as SRS dose.