PEDS: Hodgkin's Disease
Background Epidemiology and Presentation
Hodgkin's Disease represents about 6% of childhood cancers. A striking sex difference with male predominance in younger children decreasing with age. The ratio of M:F is 4:1 for 3 - 7 year olds, 3:1 for 7-9 year olds and 1.3:1 for older children and adults. There appears to be an association with EBV virus and a bimodal age distribution is demonstrated in the US and other developed nations with peaks in the 20s and 50s. It is uncommon prior to age 5 and is more common in adolescents. The role of EBV in Hodgkin's lymphoma is well established and there is evidence that non-EBV HL may have different natural history than EBV HL.
Hodgkin's lymphoma appears to be unifocal, with 90% of the patients presenting in a pattern suggestive of continuous lymphatic spread. Most children are diagnosed withn supradiaphragmatic lymph nodes are identified, with painless cervical lymphadenopath y in 80%. Mediastinal involvement is seen in 80% of the adolescents but only 1/3 of those 1 - 10 years old. Mediastinal disease can produce dyspnea, cough and SVC syndrome. Axillary lymphadenopathy is less common.
Associations between mediastinum and neck, ipsilateral neck and ipsilateral axilla, mediastium and hilum, and spleen and abdominal metastases are reported. Isolated mediastinal or infradiaphragmatic disease is rare, occuring in less than 5% of all HL patients.
About 1/3 of the patients have "B" signs as described by the Ann Arbor/Cotswold staging system.
The typical Hodgkin's Disease Presentations:
- Cervical Lymphadenopathy
- 80% present with cervical LAD
- Usually painless LAD
- Mediastinal Lymphadenopathy
- 75% present with mediastinal LAD overall, but
- among 1 - 10 year olds, only 30% present with mediastinal LAD.
- SVC syndrome
- Dyspnea
- Cough
- B signs
- About 1/3 present with "B" symptoms
- The three B symptoms are:
night sweats, weight loss, fever of unknown origin
Workup, Staging and Pathology
Workup
A careful evaluation and physical examination is vital. The location and size of all palpable nodes and Waldeyer's ring evaluation should be recorded. Patients with Stage III/IV disease or with B-signs should undergo bone marrow biopsy. Bone marrow biopsy in earlier stage disease is low yield and is not recommended.
Despite the widespread availability of CT scans, a PA chext X-ray should be obtained. This is helpful for calculating the mediastinal adenopathy bulk. CT is performed in a reclining position and will splay the mass causing an overestimation of large mediastinal adenopathy. The CT of the abdomen and pelvis should be obtained with oral and IV contrast to help discriminate structures from adenopathy.
PET/CT has significant advantages over older gallium scans in that it is more sensitive and more specific, has a higher resolution and can be performed in the same day, saving delay. PET is now recognized as an integral component of lymphoma work up.
The general workup includes the following:
- History and Physical Exam with particular attention to B signs of night sweats, fever, and weight loss
- Laboratory Studies:
- CBC/Chemistries
- ESR (sed rate)
- CRP
- LH/FSH, estradiol or testosterone levels
- Free T4/TSH
- Pregnancy Test in post-pubertal females.
- Biopsy
- Open excisional biopsy.
Avoid Core Needle or FNA biospy: The architecture should be preserved. - Supraclavicular lymph nodes are superior in sensitivity to cervical lymph nodes.
- Open excisional biopsy.
- Imaging:
- CT of the Chest/abdomen/pelvis
- CXR PA/lat
- PET or Gallium scan
- Cardiac Evaluation consisting of ECG, ECHO or MUGA (adriamycin based chemotherapy)
Staging
| I | Involvment of a single lymph node region or lymphoid structure (spleen, thymus, waldeyer's ring or single extralymphatic site) |
| II | Involvement of 2 or more lymph node region on the same side of the diaphragm or localized continuous involvment of one lymphatic region and one extranodal organ or site on the same side of the diaphragm |
| III1 | Involvement of lymph node regions on both sides of hte diphragm which may be accompanied by involvement of the spleen or localized contiguous involvement of only one extranodal organ site or both, with or without involvement of splenic hilar, celiac or mesenteric nodes |
| III2 | As above with involvement of PALN, Iliac or messenteric LN. |
| IV | Diffuse or disseminated involvement of one or more extranodal organs or tissues with or without associated nodal involvement. |
| A | No symptoms |
| B | B signs: fever > 38C; drenching night sweats; unexplained loss of > 10% of body weight in the preceding 6 months |
| X | Bulky disease (widening of the mediastinum by more than 1/3 or the presence of a nodal mass with a maximum dimension > 10 cm) |
| E | Involvement of a single extranodal site that is contiguous or proximal to the known nodal site |
| CS | clinical stage |
| PS | pathologic stage |
Nodal regions associated with HL and NHL: 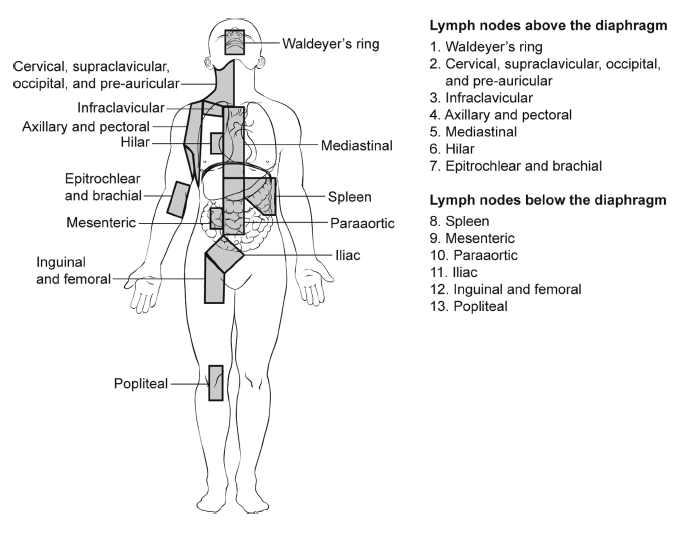
Pathology
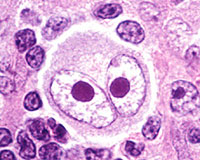
The classic pathology is the Reed-Sternberg Cell.
Excisional biopsy is preferred to preserve the lymph node architecture. FNA and CNB do not preserve architecture and may lead to missed diagnosis. Classic Hodgkin's Lymphoma subtypes (Rye Classfication) are:
- Nodular Sclerosing
- Mixed Cellularity
- Lymphocyte predominant
- Lymphocyte depleted
| Subtype | Frequency | Attributes | |
|---|---|---|---|
| Nodular Sclerosing | 44% | Most common among all age groups, but less common among children than adolescents and adults (72-77%) | lacunar variant Reed-Sternberg Cells |
| Lymphocyte Predominant | 13% | More common among children < 10 years old | CD15 Neg; CD20 Pos |
| Lymphocyte depleted | rare | ||
| Mixed cellularity | 33% | More common in children than adolescents and adults (11-17%) | ~20% have bulky mediastinal adenopathy |
Nodular lymphocyte predominant HL has a distinctive "popcorn cell" variant H&E stain. These "popcorn" cells stain for CD20 and do not stain for CD15. Classical RS cells which stain for CD15/20 are rare as is expression of EBV. Progressive transformation of germinal centers is seen, even in the absence of classic Reed-Sternberg Cells. The disease has a long smoldering course and is more common in young children. 1/3 are younger than 15 and has a high male:female predominance (4:1). It commonly involves a single lymph node, sparing the mediastinum.
Lymphocyte Rich (classic) HL cells are CD15 positive with clinical behavior similar to Mixed Cellularity HL.
Mixed Cellularity HL is CD15 positive, less common in children and can be confused with peripheral T-cell NHL. It is often accompanied by B signs and more often involves infradiaphragmatic nodes.
Nodular Sclerosiing HL subtype has collagenous bands that divide the node into nodules which often contain the lacunar variant Reed-Sternberg Cell. This disease often occurs in children ,involves the supradiaphragmatic regions and demonstrates an orderly progression along the nodal chains.
Lymphocyte depleted HL is rare and has a poor prognosis.
Risk Groups
| Presentation | Stage | Treatment Options |
|---|---|---|
| Low risk: AHOD 0431, Int. risk AHOD 0031, HR COG 59704 | ||
Early or Favorable
|
IA IIA | 2-4 cycles of Chemotherapy → low dose IFRT (21 Gy, 14 fractions @ 1.5Gy/fraction |
| Localized Unfavorable or Intermediate
|
IA, IB, IIA, IIIA | 4-6 cycles of chemotherapy + low dose IFRT 21 Gy /14 fractions |
Advanced or Unfavorable:
|
IIB, IIIB, IV | 6-8 cycles of COPP/ABVD + IFRT 21 Gy/14 fractions |
| Relapse | Low risk disease at diagnosis with relapse confined ot an area of initial involvement after chemotherapy and no RT, IFRT is used. For post-pubertal patients, standard dose RT may be used, for all other patients, induciton chemotherapy and high-dose chemotherapy with stem cell rescue is used. | |
Studies
CCG 5942 Nachman, 2002 IFRT v. Obs in CR to risk adapted chemotherapy enrolled 501 patients with CR to risk adapted combination chemotherapy randomized to IFRT or no further treatment. In an "as-treated" analysis EFS-3 was increased with IFRT from 85% to 93%, but OS-3 was unchanged at 98-99%.
GPOH-HD95 (Ruhl 2001, 2004): Risk adapted chemotherapy followed by RT depending on response to induction chemotherapy:Ruhl reported on 1018 patients treated with risk adpated chemotherapy for 2 - 6 cycles and RT with RT dose adjusted based on clinical response to treatment:
- CR: No RT
- CR: 20 Gy
- PR >75% tumor regression: 20 Gy
- PR < 75% regression: 30 Gy
- Residual tumor mass > 50 ml: 35Gy
The results of GPOH-HD95 was DFS was superior for patients given RT after PR at 92% than for no RTafter CR at 69-77%.Overall survival was unchanged at 97%. There was no advantage for low risk patients, but these results conflict with CCG5942.
Donaldson 2007: Low risk VAMP + IFRT dependant on response.110 low risk patients with VAMP x 4 cycles with IFRT: 15 Gy for CR, 25.5 Gy for PR. OS-10 was 96% EFS 89%. Toxicity: hypothyroidism in 42%, one patient with cardiac dysfuncton, two with second malignancies.
Hudson 2004: Unfavorable disease (I/II bulky, or B-signs or III/IV disease treated with alternating VAMP → IFRT (response based).Results: Trial closed early due to poor EFS. Chemotherapy was alternating VAMP/COPP → IFRT. OS-5 was 93% and EFS was 76%. Poor results are attributed to alternating chemotherapy or the ommission of radiation therapy.
AHOD 0431 low risk paitents treated with AV-PC and response based RT: If CR after 3 cycles, no RT otherwise IFRT 21 Gy in 14 cycles. Interim analysis showed EFS-1 81% for CR pn PET after 3 cycles, however increased risk of events in these patients if PET after 1 cycle is less than CR.
Toxicities
Chemotherapy toxicities:
- Bleomycin: pulmonary fibrosis/pneumontis
- doxorubicin: cardiomyopathy
- alkylators and etoposide: AML and meylodysplasia
- procarbazine: male infertility
- prednisone: avascular necrosis