Lung Cancer
Non-Small Cell Lung Cancer
Amoung the most common malignancies. Is the leading cause of cancer deaths in the world. Lung cancer is usually not diagnosed early and has an OS5 approaching 15%.
Lung cancer treatment depends on the extent of disease, location of the primary tumor and medical co-morbidities. The assessment of extra-pulmonary intrathoracic and extrathoracic disease is essential for staging and evaluation for determination of treatment.
70-80% NSCLC
NSCLC: Squamous Cell
- Central, cavitating lesions
- hypercalcemia associated
- Incidence decreasing
- least likely to metastasize to brain
NSCLC: Adenocarinoma
- peripheral
- hypertrophic, pulmonary ostesarcoma
- Dermatomyositis
- Incidence increasing/worse prognosis
- second most common metastases to brain (39%) after SCLC
NSCLC: Bronchoalveolar
- Bliateral, women predominate
- Peripheral nodule, multifocal or pneumonic adenocarcinoma arising form Type II pneumocytes
NSLCL: Large Cell
Peripheral
Natural History
- Most common non-skin cancer in the world
- 2ndmost common cancer in the US (prostate and breast)
- #1 cause of cancer death in the world and USA
- >90% caused by smoking & tobacco exposure
- Adenocarcinoma is 40-50% of NSCLC and is more often peripherally located
- BAC is an adenoCA subtype
- Squamous Cell CA is more likely to be centrally located
- Large cell like adenocarcinoma is more often peripheral and has a high tendancy to metastastize
- Carcinoid tumors are rare, tend to be endobronchial and rarely metastasize.
- about half are localized or locally advanced at diagnosis (compared to SCLC where 80% are advanced)
Lung cancers arise from either the alveolar lining cells of the pulmonary parenchyma or the mucosa of the tracheobronchial tree.
Common distant metastatic sites are:
- brain
- bones
- adrenal glands
- contralateral lung
- liver
- pericardium
- kidneys
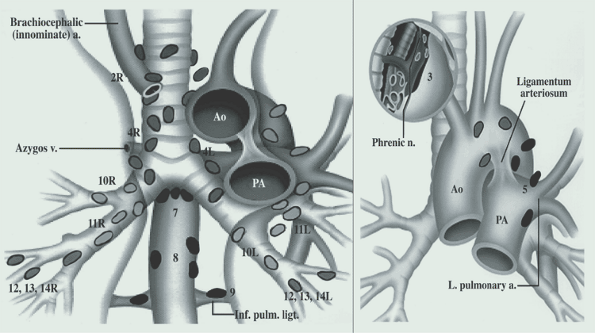
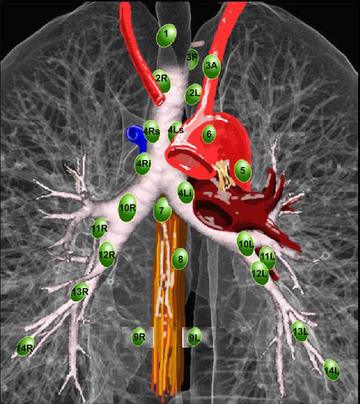
Anatomy
LUL → AP Window
- LN Stations < 10 are outside the lung
- N1 Hilar, interlobar, lobar, segmental, subsegmental
- N2 Nodal Levels
- High mediastinum
- Upper partrachial
- Pretrachial
- Lower Paratrachial
- AP Window
- PALN
- subcarinal
- paraesophageal
- Pulm ligament
High mediastinal nodes Levels 1-4. Aortic Nodes are 5-6. Inferior Mediastinal nodes are 7-9.
For intrahilar nodes, 10-14 are all intralobar and are classified as N1nodes.
Staging Workup
- HP: KPS & weight loss
- Sputum x3 80% reliable for large, central tumors, 20% for small distal tumors.
- FNA; Bronchoscopy
- Labs
- Imaging:
- CT/PET
- MRI Brain (if stage >IIB (T2N1 or T3N0) or neurologic signs)
- MRI Chest (if Thoracic Inlet tumor)
- PFTs:
- FEV1<0.8 l may be a candidate if related to tumor-- get quant V/Q
- DLCO <40% only with highly conformal RT and with close attention to V20.
- Goals for FEV1: ≥ 75% of predicted, DLCO ≥60%
- Thoracentesis if effusion: Malignant Effusion is a wet IIIB and will be a Stage IV at next staging
- Bronchoscophy for central lesions, CT guided biopsy for peripheral lesions
- Mediastinoscopy/Bronchoscopy to confirm PET/CT Positive nodes
- Mediastinoscopy to evaluate upper mediastinal (Level 1-2) nodes for all superior suclus tumors, large (T3) or central T1/T2
- Mediastinoscopy evaluates Lvl 1-2 Nodes
- Chamberlain evaluates Lvl 5-6 nodes (AP window) and differs primarily by its incision at the 3rd intercostal space instead of a cervical incision.
Syndromes
- Horner's: ptosis, partial anhydrosis, meiosis: arises from primary disease, not lymph nodes
- SVC: from Mediastinal LN. Lung cancer #1 cause, Lymphoma #2 cause
- Pancoast: Upper lobe tumor C1-T8 (brachial plexus) with ulnar pain
- Shoulder pain
- brachial plexus palsy
- Horner's Syndrome
Staging
General AJCC Principles
- Special Staging Information
- Unresectable tumors at thoracotomy should be pathologically staged
- Occult cancer (sputum positive) is staged Tx
- T2 is used with direct extension to visceral pleura
- T3 is used with direct invasion to parietal pleura
- Satelite nodules (additional small nodules) within the same lobe are T4
- --Pleural tumor foci that are separate from direct pleural invasion are also T4.
- --A separate lesion outside the paretial pleura, in the chest wall or diaphragm is metastatic M1
- --A malignant effusion is T4 and is presently classified as Stage IIIC. These cases are treated as though they are M1 disease, it is likely that the next staging revision will be a Stage IV.
- --Pericardial effusion is also T4, unless it is clearly benign. Pericardial effusion like malignant pleural effusion is a very poor prognostic indicator and is being reconsidered and may become M1 in the future.
- --Hoarseness (vocal cord paralysis) may arise from several etiologies:
- involvement of the recurrent laryngeal nerve
- SVC obstruction
- Compression of trachea or esophagus
- Usually related to N2 disease in the AP window.
- Pancoast Tumor
- Symptom complex from tumors arising in the superior sulcus
- Involves inferior branches of the brachial plexus, including the stellate ganglion.
- Classified according to standard staging.
- T4If they are:
- invading vertebral bodies or spinal canal
- encasing the subclavian vessels
- unequivocable involvement of the upper brachial plexus
T Stage
| T1 | Tumor 3 cm or less surrounded by lung or visceral pleura, without bronchoscopic evidence of bronchoscopic invasion more proximal than the lobar bronchus. A superficial tumor of any size with invasion limited to the bronchial wall which may extend to the mainstem bronchus is considered T1. |
| T2 | Tumor with any of the following features:
|
| T3 | Tumor with direct invasion of any of the following:
|
| T4 | Tumor of any size invading any of the following:
|
| N0 | No nodes |
| N1 | Mets to ipsilateral peribronchial or ipsilateral hilar nodes. Intrapulmonary nodes including involvement by direct extension |
| N2 | Mets to ipsilateral mediastinal nodes or subcarinal nodes |
| N3 | Mets to contralateral mediastinal, contralateral Hilar, or contralateral scalene or supraclavicular lymph nodes |
| M0 | No mets |
| M1 | Distant mets including separate tumor nodules in a different lobe (either ipsi-/contra-lateral |
Stage Grouping
| IA | T1 | N0 | M0 | OS1/OS5 | 90-95% / 60-80% |
| IB | T2 | N0 | M0 | 80-90% /50-70% | |
| IIA | T1 | N1 | M0 | 70-90%/ 40-70% | |
| IIB | T2 | N1 | M0 | 60-80% /30-50% | |
| T3 | N0 | M0 | |||
| IIIA | T1 | N2 | M0 | 40-70% / 20-30% | |
| T2 | N2 | M0 | |||
| T3 | N1 | M0 | |||
| T3 | N2 | M0 | |||
| IIIB | Any T | N3 (contralateral) | M0 | 10-40%/ <5-10% | |
| IV | M1 | MS 3-6 months with best supportive care, 8-10 mo. with chemo |
.