Hodgkin's Lymphoma
Background
There are about 7,500 new cases of Hodgkin's Lymphoma in the US each year. There is a bimodal distribution with peaks at age 25 years and at age 60 - 70 years. The second peak of the curve is much smaller than the earlier peak. Most of the disease occurs in younger patients. A number of studies have suggested a genetic predisposition for HL with a note of increased incidence in Jews and amoung first degree relatives.
There are two broad categories of HL: Classic (more common) and Nodular lymphocyte predominant HL (NLPHL).
Classic Hodgkins Lymphoma has four subtypes:- Nodular Sclerosing (most common type in US)
- Mixed Cellularity
- Lymhocyte depleted (worst prognosis)
- Lymphocyte rich (best prognosis)
Classic Hodgkin's Lymphoma are typically CD15 and CD30 positive and CD 45 and CD20 negative. Hodgkins Lymphoma consists of Reed-Sternberg Cells,
The most common presenting lymph node regions a initial diagnosis vayr by cell type. Cervical chains account for 70% of all patients, followed by Mediastinum with around 50%. Patients who present with mediastinal adenopathy most commonly have nodular sclerosing classic HL. Those with cervical chains
Nodular sclerosing HL is the most common Hodgkin's Lymphoma and is frequently found in the mediastinum.
Lymphocyte depleted HL is more commonly seen in older age and in HIV+ patients.
Nodular Lymphocyte Predominant HL (NLPHL) carries a greater risk of subsequent development of a non-Hodgkin's Lymphoma. Nodular lymphocyte predominant HL (NLPHL) has different markers than Classic HL. NLPHL is typically CD15 and CD30 negative but CD45 and CD20 positive which is the reverse of classic HL and more akin that of Non-Hodgkin's lymphomas.
Patients may present with B symptoms. B symptoms include:
- Fevers > 38C
- > 10% body weight loss in 6 months
- Drenching night sweats.
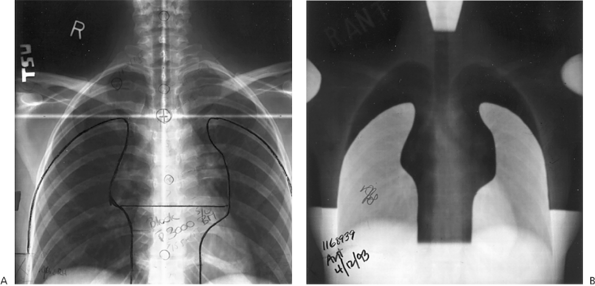
Hodgkin's Disease can be described as bulky. Bulky disease in the mediastinum has been defined as mass > 1/3 the intrathoracic diameter at T5-T6 on upright PA chest Xray. Disease outside of the mediastinum has variable definitions based on investigator preference most often being described as a mass > 5 cm or a mass > 10 cm.
 |
Workup and Staging
In the usual fasion, H&P with emphasis on adenopathy, B-signs: fever, drenching night sweats and weight loss. Laboratory studies including ESR CBC, albumin and LDH levels. Labs necessary for RT treatment planning include BUN, Creatinine and βHCG level in women of childbearing years. HD can also present with alcohol induced pain and puritis, but most commonly it presents with painless adenopathy. A comprehensive nodal examination is necessary.
Bone marrow biopsy is indicated in disease that may be advanced:
- B-signs
- Stages III - IV disease
- Bulky Disease
- > 2 sites
- Recurrent disease
Tissue diagnosis is necessary. Excisional biospy is the standard to preserve nodal architecture, which is important in the diagnosis FNA and to a lessor extent core needle biopsy do not preserve architecture, although CNB is being used more commonly than in the past.
Staging PET/CT exams are typically used twice: once prior to treatment as part of the staging workup and once after completion of initial chemotherapy to assess response to treatment.
Staging
Hodgkins Lymphoma is staged according to the Ann Arbor Staging System:
| I | Involvement of 1 Nodal region or a single extra-lymphatic organ |
| II | Involvement of ≥ 2 LN regions on the same side of the diaphragm or localized involvement of a single extralymphatic organ and its regional lymph nodes ± involvement of other LN regions on the same side of the diaphragm |
| III | Involvement of LN regions on both sides of the diaphragm that may also be accompanied by localized involvement of an associated extra-lymphatic organ or site |
| IV | multifocal involvement of ≥ 1 extralymphatic organ involvement ± associated lymph nodes or isolated extralymphatic organ involvement with distant nodal involvement |
| ModifiersPatients without B signs are "A" and with B signs are "B". Patients with extralymphatic organ involvement are "E" Spleen and Waldeyer's Ring are considered lymphatic organs and therefore are not staged with an "E" suffix. Spleen involvement is "S" and bulky adenopathy is "X" | |
The 2010 AJCC Staging system considers Bone marrow, liver, pleura and CSF to be Stage IV disease.

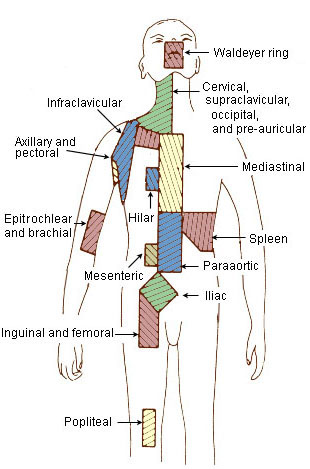
Regional lymphatics are defined by the "Rye" classification. The Rye Classification predates the Ann Arbor Staging system. The Rye definition of regional lymphatics remains unchanged.
 |
 |
The RYE Classification of nodes:
| |
Prognosis Factors
Risk factors for early stage Hodgkin's Lymphoma vary, based on trials. Some more common unfavorable risk factors are:
- age ≥ 50 years
- Bulky disease (various definitions of > 5, 8 cm or > 1/3 mediastinal width)
- ≥ 4 sites
- ESR > 50 (No B-signs), ESR > 30 (With B-signs)
- Presence of extranodal sites
- Mixed cellularity or lymphocyte depleted histologies
International Prognostic Score (IPS) for HD lists a number of unfavorable factors for advanced Hodgkins' Lymphoma:
- WBC >15,000
- Albumin < 4
- Lymphocytes < 600
- Stage IV disease
- Hb < 10.5 g/dL
- Age ≥ 45 years
- Male gender
- WALSH AM
| Subtypes | Relative Frequency | 5 Year Survival | Stage at Dx | B Symptoms at Dx |
| Lymphocyte predominant | 5-l0% | 90% | 90% PS I-II | 4% |
| Nodular sclerosis | 50-70% | 80% | 60% PS I-II | 34% |
| Mixed cellularity | 20-30% | 50-60% | 54% PS III-IV |
37% |
| Lymphocyte depleted | <5% | 20% | 77% PS III-IV | 73% |
Early stage disease treated with chemo-RT have a 5 year Freedom from failure of 95% and OS > 95%. About 30% of early stage favorable disease have occult splenic involvement.
Advanced stage disease : if ≤ 3 IPS factors, then FFP-5 is 70%. The 5 years freedom from progression drops to 50% if > 3 IPS adverse factors are present.
Staging laparotomy was historically performed as part of the HL workup. This included a liver biopsy, splenectomy and abdominal lymph node sampling. A European study, EORTC H6F (Carde, 1993 JCO) demonstrated that staging laparotomy is unnecessary. The elements of this study:
- Included favorable Stage I/II patients with supradiaphragmatic disease
- Randomized:
- Staging laparotomy with treatment based on staging laparotomy results
- OR Clinical staging only with sub-total nodal irradiation (STNI).
- STNI includes (per Hansen 2nd Ed), total lymph irradiation with the exclusion of the pelvic fields.
- FFP-6 was unchanged at 78% - 83% as was OS-6 at 89% - 93%.
- There was no difference in outcomes between the two arms; Staging laparotomy is not needed.
Treatment and Prognosis
Radiation therapy was the earliest treatment of Hodgkins' disease. Xrays were used as early as 1901 at the end of the 19th Century. In the early 20th century, fractionated and single fraction RT shrunk adenopathy but did not control the disease and fell out of favor as subsequent treatments were less effective as radiation resistance developed. In 1920, a Swiss radiotherapist Gilbert, advocated treating adjacent nodal chains suspected of harboring sub clinical disease. Peters at PMH reported in the late 1930s/early 1940s survival rates of 79% at 10 years for limited stage HL. Prior to this report, 10 year survival was nearly zero.
With the advent of chemotherapy, significant clinical response was seen, but relapse rates were seen in almost all cases, and cure was not achievable with chemotherapy alone. Radiation remains an integral component of HL treatment. RT fields have been described in many ways, which might lead to confusion. Per DeVita, the following are standard descriptors of radiation fields:
Standard Radiation Fields Used in HL
- IFRT: Involved field RT: limited to the site of the clinically involved nodal field based on the Rye Classification.
- neck (unilateral cervical/supraclavicular ln)
- mediastinum (including hilar/supraclavicular regions bilaterally)
- axilla including supraclavicular and infraclavicular LN
- para aortic LN (± spleen)
- Inguinal (including ilac and femoral LN
- TNI: Total nodal irradiation: Covering all nodal areas with mantle and inverted Y fields
- STNI: Excluding spleen and pelvic (iliac and femoral) groups.
Other definitions of RT fields include:
- IFRT: involved fields as described by the Rye classification
- RFRT covers involved regions + immediately adjacent regions (regional nodal RT)
- INRT: only the pre-chemotherapy tumor volume. Currently under investigation in European trials.
Chemotherapy
The most common chemotherapy multi-agent regimens are:
- ABVD (a big vial of drugs): Adriamycin, Bleomycin, Vinblastine, Dacarbazine
- Stanford V (MOPE-ABV): Mechlorethamine, Vincristine, Prednisone, Etoposide, Adriamycin, Bleomycin, vinblastine.
- Dose Escalated BEACOPP: Bleomycin, Etoposide, Adriamycin, cyclophosphamide, vincristine, procarbazine, prednisone.
BEACOPP is more commonly used in advanced stage HL more frequently in Europe than in the US.
Treatment Paradigms
There are treatment paradigms for various stages and cytologic subtypes of HL based on IPS favorable and unfavorable categories;
Stage I-IIA Favorable Classic HL
Common strategies include:
- Chemotherapy + planned IFRT
- ABVD x 4 cycles ± IFRT to residual PET positive sites at restaging
Stage I-II unfavorable classic HL:
- Chemotherapy + planned IFRT
- ABVD x 6 Cycles ± IFRT to initial bulky disease and/or residual PET/CT positive sites at restaging.
Stage III-IV Classic HD:
- ABVD x 6 - 8 cycles ± IFRT to initial bulky disease and/or residual PET positive areas at restaging
- Stanford V (MOPE-ABV) + IFRT to initial bulky disease and PET + residual sites.
- Dose escalated BEACOPP + IFRT to initial bulky disease and PET + residual sites.
Stage I - II Nodular Lymphocyte Predominant Hodgkins Lymphoma (NLPHL)
Stage I = II NLPHL can be treated similarly to low grade HL. This stage can be treated with IFRT or RFRT alone (no chemotherapy). IF B-signs are present, treat with chemotherapy + IFRT.
Stage III-IV NLPHL
Stage III-IV NLPHL can be treated with observation, definitive Chemotherapy ± RT or palliative chemotherapy or radiotherapy.Radiation Therapy
Radiation therapy fields are: IFRT, RNRT, TNI, STNI. Common doses to IFRT after initial chemotherapy are 30.6 Gy. Additional dose to 36 Gy is commonly added for bulky disease sites.
Evidence suggesting improved outcomes combining chemotherapy and radiation therapy in HL come from four major randomized trials:
- EORTC H7F 2006 JCO
- EORTC H8F 2007 NEJM
- German HD7 2007 JCO
- SWOG S9133 2001 JCO
Chemotherapy and radiotherapy varied in these studies. Despite this variation, long term relapse rates consistently favored chemo/RT. In the H8F trial, OS-10 was significantly improved with chemo/RT but long term OS was similar to other studies.
Evidence Concerning Elimination (or not) of consolidating RT after CR to chemotherapy in HL
There have been at least 3 major randomized controlled trials which have evaluated chemotherapy alone in early and advanced HL.
NCIC-Canada/ECOG Unfavorable, Non-bulky Stage I-II HL (Meyer 2005 JCO):
- Randomized unfavorable, non-bulky, Stage I/II to
- ABVD x 4 - 6 cycles (or 4 cycles if CR after 2 cycles)
- ABVD x 2 cycles → STNI.
- FFP-5 (freedom from progression at 5 years) favored Chemo/RT arm at 95% over 88%
- OS not significantly different at 92% for CRT over 95% for ABVD alone.
- Authors suggest lack of OS benefit was due to increased toxicity of the combined modality group, and a difference favoring ABVD may be seen in the long term, due to late RT toxicity.
Lasker Randomized a diverse cohort of patients in India Stage I-IV ± bulky disease and/or B-signs, adults and children who had CR after 6 cycles of Chemotherapy (ABVD x 6)
- Randomized to IFRT or observation
- A majority of patients had mixed cellularity (the most common in India).
- IFRT improved EFS-8 from 76% to 88% and OS-8 from 89% to 100%, especially in patients < 15 years old with B-signs, bulky disease and advanced stages.
Aleman Randomized Stage III-IV HL who had CR after 4 or 6 cycles of MOPP-ABV to IFRT or observation (2007 IJROBP)
- Patients who had CR after 2 cycles received 4 cycles of MOPP-ABV.
- Patients who had CR after 4 cycles received 6 cycles of MOPP-ABV.
- There was no difference in EFS-8 at 77% compared with IFRT 73%
- There was no difference in OS-8 at 85% compared with IFRT at 78%
EORTC H10 is an ongoing trial comparing ABVD alone in patients who have a complete response on PET/CT after 2 cycles of ABVD to ABVD + INRT.
IFRT or More Extensive RT?
At least 4 randomized trials have compared IFRT to more extensive radiation in Hodgkins disease patients receiving chemo-radiation therapy. The 5 - 12 year OS outcomes were similar in all of these trials suggesting that more extensive RT than IFRT was unnecessary.
- Groupe Pierre et Marie Curie (GPMC JCO, 1985)
- German HD 8 (Kilmm 2007 Ann. Oncol.)
- Milan Study (Banadonna 2004 JCO)
- EORTC H8U (Ferme C, 2007 NEJM)
Can IFRT dose be reduced after induction chemotherapy?
The use of < 30 Gy in favorable stage I/II HL after intial chemotherapy has been studied in at least 2 RCTs.
HD10 German Hodgkin Study Group (Engert 2010 NEJM)
- Randomization 1:
- 2 cycles of chemotherapy
- 4 cycles of chemotherapy
- Randomization 2:
- IFRT to 20 Gy
- IFRT to 30 Gy (2 x 2 factorial design)
- PFS-5 from Treatment failure and OS were similar between the chemo comparison and the RT dose comparison
EORTC GELA H9F Study randomized favorable Stage I-II HL with CR after EBVP (Noordijk 2005 Abstr. ASCO:
- Favorable Stage I-II HL treated with EBVP (epirubicin,bleomycin,vincblastine, prednisone) x 6 cycles
- If CR then Randomize:
- 36 Gy IFRT
- 20 Gy IFRT
- NO IFRT
- EFS-4 was similar between 36 Gy and 20 Gy arms, at 87% and 84% but was significantly worse in no IFRT arm at 70%
Consolidation RT appears to be more important in Stanford V (MOPE-AVB) chemotherapy regimen
Two randomized studies have examined ABVD and Stanford regimens for HL:
ABVD compared with Stanford V (Gobbi 2005 JC) Gobbi reported that RT was not necessary and was only used in 2/3 of the Stanford V arm and 62% of the ABVD arms. FFS-5 significantly favored ABVD at 78% compared with Stanford V at 74%.
Hoskin Randomized trial of unfavorable HL Stage I-II and Stage III-IV HL to ABVD or Stanford V (2009 JCO): Initially IFRT wa required to a site initially > 5 cm but in the latter parts of the study, RT was optional for the ABVD arm. Ultimately 53% in the ABVD arm and 74% in the Stanford V arm received IFRT. Despite the higher rate of consolidation RT in the Stanford V arm, the PFS-5 was 76% in ABVD arm and 74% in the Stanford V arm. OS was not significantly different between the two arms.
PORTS
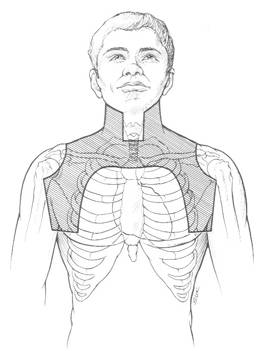
Mantle Field:Classic HL port covering all nodes above the diaphragm from T10-T11 to the low neck.
MIni-mantle field:Reduced mantle field omitting mediastinal, hilar and neck nodal regions.
modified mantle field: mantle field which omits neck and axilla fields
TLI/TNI:mantle field plus PALN and PLN -- Inverted Y + spleen
STLI: TLI excluding pelvic LN.
Block the larynx throughout unless there is midline disease. Block the larynx after 20 Gy in that case. A subcarinal block is used to block the heart. Consider blocking after 15 Gy in those who have had complete response after induction chemotherapy , otherwise block the heart after 30 Gy.
 |
 |
 |
TNI includes mantle, PALN,
Toxicity
Late second malignancy risk 30 years post treatment is 2-3 times the general population for those who survive > 5 years.
Leukemias tend to occur < 5 years after treatment; solid tumors > 7 years after treatment.