Meningioma
Background
Menigiomas are the most common benign CNS primary tumor. They are second only to gliomas in frequency with 15% - 20% of all primary intracranial tumors. Meningiomas generally appear late in life, in the 7th decade with a female preponderance by 2:1.
Risk factors associated with the development of meningiomas include:
- Prior Radiation (RR 10)
- NF-2
- Hormone replacement therapy -- meningiomas have PR receptors (RR 2)
NF-2 protein defect is merlin. NF-2 also predisposes to acoustic neuromas, ependymomas and juvenile subcapsular cataracts.
About 75% of Grade I meningiomas express progesterone receptors.
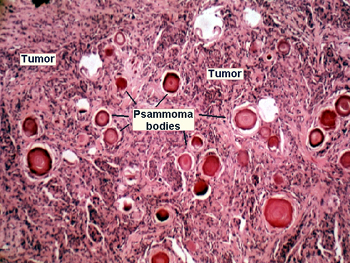
Microscopically, meningiomas contain psammoma bodies and calcifications.
 |
Negative Prognostic factors for mengiomas:
- High Grade
- Young age
- Chromosome alternations
- Poor performance status
- Subtotal resection
Workup and Staging
Meningiomas are claissified by WHO grades. The WHO grades are:
- WHO Grade I: benign
- WHO Grade II: atypical, clear cell, chordoid
- WHO Grade III: anaplastic/malignant, rhabdoid, papillary
Surgical Grading is based on extent of resection and is known as the Simpson Grade: Grade I = GTR . . . Grade IV: STR. The Simpson grade predicts the likelihood of recurrence locally. 80% achieve a gross total resection. GTR is more difficult or impossible in the cavernous sinus, petroclival region, post sagital sinus, and optic nerve.
90% of all meningiomas are Grade I. The remainder are Grade II at 6% and Grade III at 4%.
Optic sheath meningiomas are diagnosed from imaging or clinically by a neuro-radiologist. No biopsy is attempted.
Angioblastic subtype meningioma is the most aggressive grade I meningioma.
The overall survival difference between Grade II and Grade III menigniomas (atypical v. malignant) is 12 years for atypical Grade II compared with 3.3 years for Grade III meningiomas (anaplastic).
Prognostic factors for anaplastic meningioma include brain invasion, adjuvant RT, extent of resection, and p53 overexpression.
Headache is the most common presenting sign. Meningiomas appear homogeneously enhancing ± dural tails on CT and MRI. About 60% of meningiomas exhibit a dural tail. Other diseases exhibiting a dural tail inlcude chloroma , lymphoma and sarcoidosis.[Chloromas are green collections of lymph cells associated with AML and MM. they can occur in any organ and CNS involvement is rare. They are treated with chemotherapy and surgery/radiation if persistent.]
The majority of meningiomas are found incidentally remain stable on serial imaging. This accounts for about 2/3 of the meningiomas discovered. Slower growth rates are found in the elderly and in those with calcifications.
Treatment
The general meningioma paradigms are:
- Incidental and assymptomatic finding: OBSERVE
- Grade I symptomatic and/or progressive: surgery ± RT
- Grade II or III: Surgery + RT.
- If site is surgically inaccessible (optic sheath and cavernous sinus) RT is primary modality.
- Observation should be considered with incidental/asymptomatic and stable lesions.
Radiation is used after surgery generally in a delayed fashion if there is recurrent disease. Radiation is also indicated in the event of a subtotal resection, or if there is atypical/anaplastic histology or brain invasion.
Recurrence rates after surgery alone are about 10% in GTR and 40% after STR. There is controversy surrounding the need for immediate (up front) radiation therapy after subtotal resection. Immediate post-operative radiation rates are equivalent to salvage rates. Data from an ongoing RCT (EORTC 26021) is not yet published.
Radiation Therapy
Radiation doses are 54 Gy for benign meningiomas and 60 Gy for malignant meningiomas. The PTV=GTV+1.5 cm. There is radiation dose response data for meningiomas. Goldsmith reported improved PFS with doses > 53 Gy in 1994.
Typical SRS doses range from 12 Gy - 16 Gy to the 50% IDL (in γ-knife devices) to the tumor margin depending on location and size. The 5 year local control rate is 98%. LC-5 is worse in men and if the RT dose is < 12 Gy. Male gender is associated with worse outcomes. If possible, the dural tail should be included in the GTV. Some studies have demonstrated improved outcomes (better DFS-5 if the dural tail can be included.
Toxicity
The surgical complication rate after resection for meningioma is 2% - 30%, depending on location and type. 1% - 14% mortality which is worse in the elderly.
If observation is elected, serial MRIs should be obtained at 3 months, 9 months and then yearly if stable.
SRS Toxicity is seen in doses above 16 Gy. There is temporary toxicity in 10% and permanent toxicity in 6%. Perilesional edema is seen in 15%.
The chiasm should be limited to ≤ 8 Gy with SRS..
Cavernous sinus, and optic nerve sheath tumors are followed with serial MRIs and neuro-opthalmology exams and regular endocrinology studies.
As with most radiation induced second tumors, the latency period is approximately 20 years from RT exposure to the development of a meningioma.
Meningiomas recur an average of 4 years after initial surgery.