CNS Background
General CNS Neoplastic Processes
There are about 50,000 - 55,000 cases per year of CNS tumors. The most common of these are brain metastases from other sites. 20% - 40% of all cancer patients develop brain metastases and that number is increasing as we are increasingly able to control cancer locally, regionally, and systemically.
CNS Primary Tumors
The most common type of brain primary tumors are
- Gliomas involving about 40%
- Meningiomas involving 15% - 20%
The most common malignant CNS tumor in children is a juvenile pilocytic astrocytoma (JPA) which is a WHO Grade I tumor. These tumors are 20% of all brain tumors in those under 14 and 12% in those over 14 years.
The most common histologic malignant adult CNS tumor is a high grade glioma, mostly glioblastoma multiforme. Adult tumors are primarily high grade gliomas with high grade gliomas reacing 75%. The remainder are low grade (WHO Grade I/II) at 25%.
The strongest risk factor for developing primary CNS tumors is ionizing radiation in children. There is no known threshold dose. The frequency is glioma, meningioma and nerve sheath tumors.
Genetics
Certain genetic syndromes are associated with primary CNS tumors. These syndromes and some tumor characteristics are:
| Genetic Syndrome | Disease | Histopathology |
|---|---|---|
| NF-1 |
|
|
| NF-2 |
|
|
| Tuberous Sclerosis |
|
|
| Von Hippel-Lindau | Hemangioblastoma | |
| Li-Fraumeni | Glioma | |
| Cowden | Meningioma | psamomma bodies |
| Gorlin | medulloblastoma | |
| Turcot | medulloblastoma and glioblastoma | |
| RB (retinoblastoma) | pineoblastoma | Flexner-Wintersteiner rosettes |
| Ataxia Telangiectasia | CNS lymphoma | |
| MEN 1 | Pituitary Adenoma |
Histology
Primary CNS tumors are graded using WHO criteria. WHO criteria are microscopic criteria and are based on the finding of the following features:
- Nuclear Atypia
- Cellularity and Mitosis
- Endothelial Proliferation
- Necrosis
Gliomas common overespress EGFR receptors up to 30% - 50% in GBM. PDGFR is expressed in non-GBM CNS primary tumors. Neural stem cells express the CD133 marker and are thought to be a precursor for astrocytomas. p54 is frequently lost in low and high grade gliomas. p53 is on chromosome 17.
NF-1's genetic mutation is 17q11.2/neurofibronin. This mutation predisposes optic and intracranial gliomas.
Workup and Staging of Brain Tumors
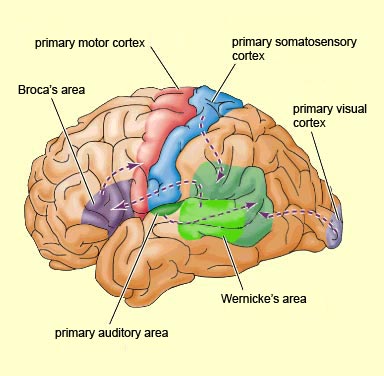
Most brain tumors produce signs and symptoms related to mass effect in the brain. They produce physical signs in relation to the neuranatomy and functon of the area they are impacting. For this reason, a knowledge of functional anatomy is helpful to understand the neoplastic process.
Functional Anatomy of the Brain and Skull
Speech centers are in the dominant left frontal lobe. The area of speech expression is called Broca's area. The dominant/left temporal lobe is associated with Wernicke's area or receptive aphasia.
 |
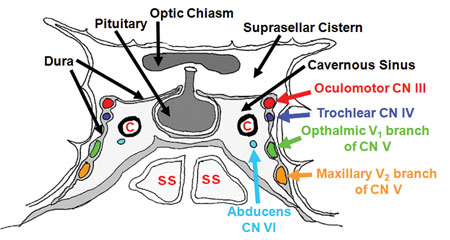
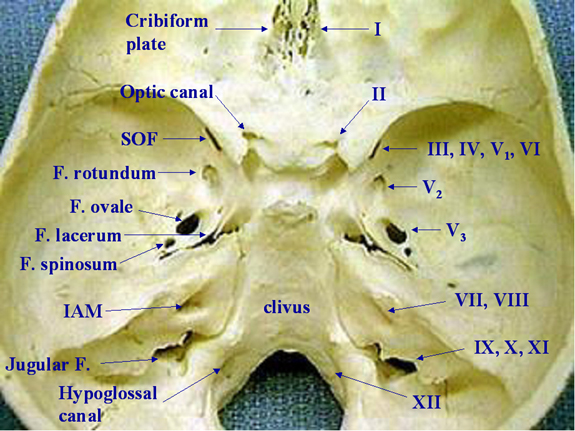
Cranial Nerve Associations/Base of Skull
CSF is formed in the choriod plexus which is produced in the floor of the ventricles.
The cavernous sinus carries occulomotor nerves CN III, IV, VI and the trigeminal V.1 and V.2 nerves. It allso carries the internal carotid artery. If a tumor involves the cavernous sinus it will commonly affect the abducens nerve causing a 6th nerve palsy resulting in a loss of lateral gaze in the affected eye. The clinical syndrome will be an eye that looks straight ahead when the gaze is averted to the affected side, resulting in a disconjugate gaze, or no abduction of that eye.
 |
The superior orbital fissure involves cranial nerves III, IV, VI and V.1
The foramen rotundum serves as the passage for V.2
The foramen ovale passes V.3 (down in the valley, under the rotundum)
The internal auditory meatus passes CN VII/VIII.
The Stylomastoid foramen passes the CN VII where it emerges from the skull.
The Jugular foramen passes IX-XI.
 |
There are 31 spinal nerves broken down as follows:
- 8 cervical nerves
- 12 thoracic nerves
- 5 lumbar nerves
- 5 sacral nerves
- 1 coccygeal nerve
The spinal cord ends at L3-L4 in children and L1-L2 in adults. The thecal sac ends at S2-S3 in both children and adults. There are several dural tail tumors that cause the "dural tail sign." The most common is meningioma 60% of the time, but others include chloroma, lymphoma, and sarcoidosis.
Toxicity of Treatment
Most common brain treatment toxicities include alopecia, dermatitis, fatigue, transient worsening of neurologic symptoms, including nausea and vomiting, otitis externa, seizures and edema (usually temporary).
Somnulence syndrome appears 6 - 12 weeks post radiation therapy due to transient axonal demylination.
Late CNS compications are serious and potentially life threatening. They include radionecrosis, leukoencephalopathy, retinoplathy, cataracts, endocrine deficits, memory loss, learning dficits, and hearing loss. The timing of late effects is 3 months to 3 years.
Prognosis Factors
Recursive Partition Analysis: RPA Classes and Life Expectancy
The recursive partition analysis pre-temazolomide was divided into 6 categories:
| RPA Categories for Malignant Gliomas -- (Pre-Temozolomide) | ||||
|---|---|---|---|---|
| Class | Characteristics | Median Survival (mo.) | OS-1 | OS-5 |
| I |
|
59 months | 90% | 76% |
| II |
|
37 mo. | 85% | 68% |
| III |
|
18 mo. | 70% | 35% |
| IV |
|
11 | 45% | 15% |
| V |
|
9 | 30% | 6% |
| VI |
|
5 | 20% | 4% |
RPA Classification for Malignant Gliomas (Survival with Temozolomide)
| Class | Characteristics | Median TMZ/RT Survival | OS-2 |
|---|---|---|---|
| III |
|
21 mo. (v. 15 mo.) | 43% (v. 20%) |
| IV |
|
16 mo. (v. 13 mo.) | 28% (v. 11%) |
| V |
|
10 mo. (v. 9 mo.) | 17% (v. 6%) |